Women’s health is a field marked by continuous innovation, where new technologies regularly redefine standards of care and training. One such groundbreaking development is the Gynecube, a sophisticated tool that is transforming how medical professionals learn, practice, and perfect gynecological procedures. It represents a significant leap forward, moving critical training from high-pressure real-world scenarios to a controlled, risk-free environment. This guide will explore the multifaceted world of the Gynecube, from its role as a training simulator for surgeons to its application as a personal device for pelvic health management.
We will delve into what the Gynecube is, how its different forms work, the benefits it offers for patient safety and personal wellness, and its growing importance in modern healthcare. This comprehensive look will demystify the technology and highlight its profound impact on both medical professionals and the women they care for.
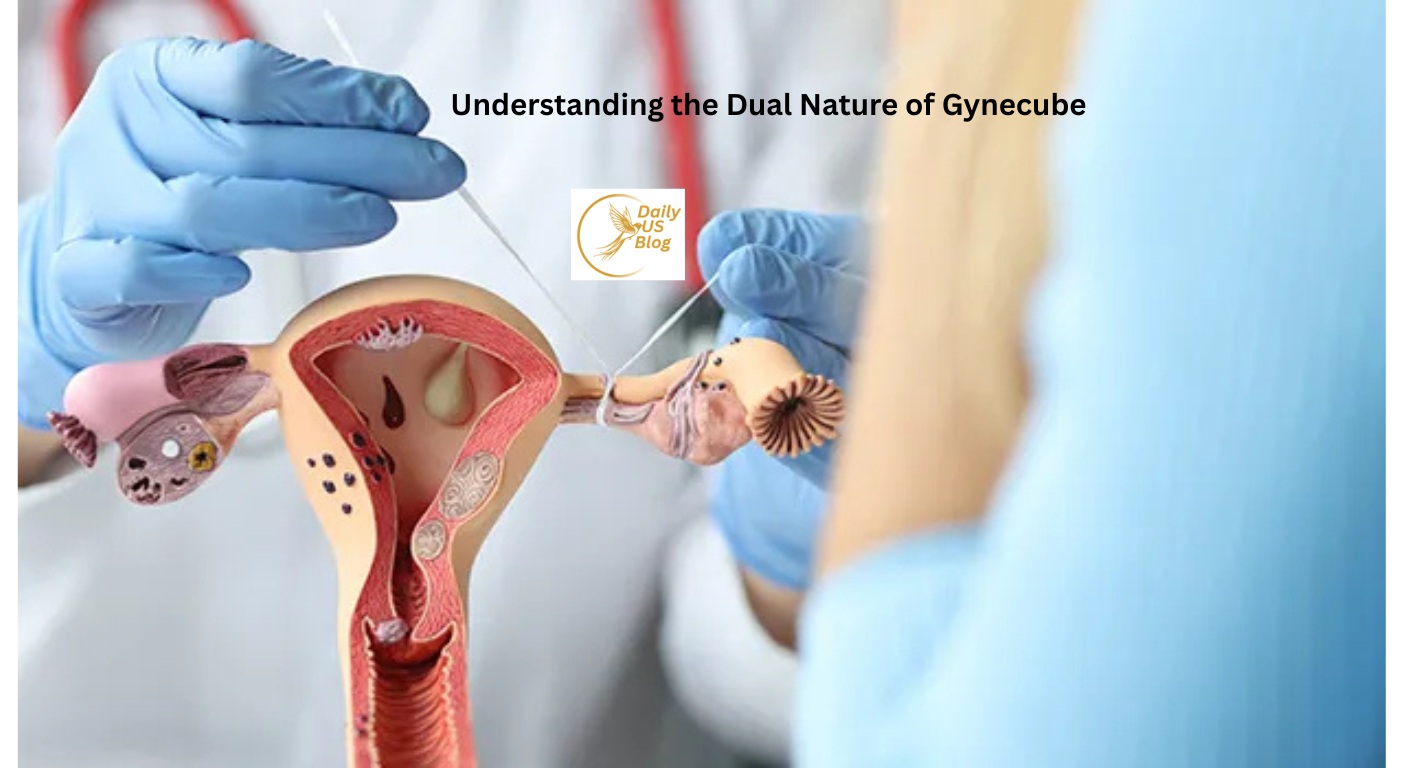
Understanding the Dual Nature of Gynecube
The term “Gynecube” has emerged in two distinct but related contexts within women’s health, which can cause some confusion. On one hand, it refers to a highly advanced medical training simulator. On the other, it describes an innovative personal device for managing pelvic prolapse. Understanding both is key to appreciating its full impact.
The Gynecube as a Medical Training Simulator
At its most complex, the Gynecube is a state-of-the-art medical simulator designed for gynecologists and surgeons in training. Think of it as a flight simulator for the operating room. It provides an incredibly realistic, anatomically correct model of the female pelvic region. This allows medical students, residents, and even experienced surgeons to practice a wide range of procedures without any risk to a live patient.
This version of the Gynecube combines lifelike physical models with advanced software and haptic feedback. This technology provides tactile sensations, allowing the user to “feel” the resistance of tissue or the subtle feedback from surgical instruments. This hands-on experience is crucial for developing the muscle memory and delicate touch required for intricate gynecological surgeries.
The Gynecube as a Personal Pelvic Health Device
In a different application, the Gynecube is an innovative, non-invasive device designed to support women experiencing pelvic organ prolapse. This condition occurs when the muscles and ligaments supporting the pelvic organs weaken, causing them to drop or press into the vagina.
This personal Gynecube is made from soft, flexible, medical-grade materials. It is designed to be inserted into the vaginal canal to provide gentle support to the weakened pelvic floor muscles. By doing so, it helps alleviate the discomfort and symptoms associated with prolapse, allowing women to regain comfort and confidence in their daily activities. It offers a practical and discreet alternative to more invasive treatments like surgery or traditional pessaries.
The Gynecube Simulator: Revolutionizing Gynecological Training
Medical simulation now plays a vital role in training the next generation of healthcare professionals. The older model of “see one, do one, teach one” contributed valuable lessons but also exposed patients to avoidable risks during a surgeon’s learning phase. The Gynecube simulator transforms this process by enabling consistent, hands-on practice in a protected environment.
Core Features of the Training Simulator
The power of the Gynecube training system lies in its sophisticated components working in harmony to create an immersive learning experience.
High-Fidelity Anatomical Models
The simulator’s foundation is its anatomically precise pelvic model. Crafted from materials that mimic the texture and feel of human tissue, it includes detailed replicas of the uterus, ovaries, cervix, and other structures. Instructors can even introduce various pathologies, like fibroids or polyps, to create diverse training scenarios.
Advanced Haptic Feedback
Perhaps the most groundbreaking feature is haptic feedback. When a trainee uses a surgical tool within the simulator, the system generates realistic force feedback. They can feel the tension of a suture or the resistance of tissue, which is vital for developing the fine motor skills needed for minimally invasive surgery. Without haptics, a simulator is just a visual exercise; with it, the Gynecube becomes a true skills-development tool.
Integrated Software and Performance Metrics
A powerful software program runs the simulations and tracks every aspect of the user’s performance. It records metrics such as time to completion, efficiency of movement, instrument precision, and the amount of force applied. After each session, the Gynecube provides a detailed report with objective data, helping trainees identify strengths and weaknesses far more effectively than subjective observation alone.
Key Procedures Practiced on the Gynecube
The simulator’s modular design allows it to be used for a wide spectrum of gynecological procedures, making it invaluable for comprehensive training.
|
Procedure Type |
Description |
Skills Developed |
|---|---|---|
|
Diagnostic Hysteroscopy |
A minimally invasive technique used to visually inspect the uterine cavity and identify potential sources of abnormal uterine bleeding. |
Camera navigation, visual identification of pathologies, instrument handling. |
|
Operative Hysteroscopy |
The removal of abnormalities like polyps or fibroids from the uterine cavity. |
Tissue resection, use of energy devices, precision cutting. |
|
Laparoscopic Skills |
Basic training for minimally invasive surgery, including camera work and suturing. |
Hand-eye coordination, depth perception, ambidextrous instrument use. |
|
Salpingectomy |
Surgical removal of a fallopian tube, often performed for an ectopic pregnancy. |
Tissue dissection, controlling bleeding (hemostasis), organ manipulation. |
|
Ovarian Cystectomy |
A surgical technique that carefully removes a cyst from the ovary while keeping the ovary intact and functioning. |
Delicate tissue handling, precise dissection, and suturing techniques. |
The Personal Gynecube: A New Solution for Pelvic Prolapse
For millions of women, pelvic organ prolapse is a challenging condition that affects quality of life. The personal Gynecube device offers a promising, non-surgical approach to managing its symptoms.
How the Personal Prolapse Device Works
The personal Gynecube is designed for comfort and ease of use. It is inserted by the user into the vaginal canal, where its ergonomic shape provides support to the pelvic organs. This helps to reduce feelings of pressure, bulging, and discomfort.
- Support and Stability: It gently holds the pelvic organs in a more natural position, alleviating the direct symptoms of prolapse.
- Comfort and Discretion: Made from a soft, flexible material, it adapts to the body’s contours, allowing it to be worn comfortably throughout the day during various activities.
- Empowerment: It gives women a tool to manage their condition proactively and privately, enhancing their sense of control over their bodies.
Benefits Over Traditional Methods
Compared to traditional treatments, the personal Gynecube offers several distinct advantages.
- Non-Invasive: It provides an alternative to pelvic reconstructive surgery, which comes with surgical risks and a lengthy recovery period.
- User-Friendly: Unlike traditional pessaries that may require fitting and insertion by a healthcare provider, the Gynecube is designed for easy self-management.
- No Hormones or Medication: It is a mechanical solution that does not rely on pharmaceuticals, avoiding potential side effects.
- Improved Quality of Life: By reducing symptoms, women often report being able to return to activities they previously avoided, such as exercise or social engagements, leading to improved confidence and well-being.
The Future of Gynecology is Integrated
Whether as a training tool or a personal health device, the Gynecube is a clear indicator of the future of gynecology—one that is more precise, less invasive, and deeply patient-centric.
The simulator version of the Gynecube ensures that the next generation of surgeons is better prepared than ever before. It standardizes training, improves surgical outcomes, and ultimately enhances patient safety by moving the learning curve out of the operating room. As surgical techniques become even more advanced, with robotics and AI playing larger roles, simulation platforms like the Gynecube will become indispensable.
Simultaneously, personal devices like the prolapse-support Gynecube empower women to take an active role in managing their health. This trend toward patient-led care and accessible, at-home solutions is reshaping how we approach chronic conditions. The development of such a thoughtful product signifies a deeper understanding of women’s needs and a commitment to providing solutions that fit seamlessly into their lives. The ongoing innovation in products like the Gynecube is crucial for advancing women’s health.
Frequently Asked Questions (FAQs)
1. What is the primary purpose of a Gynecube?
The term Gynecube is used for two main innovations. The first is a medical simulator for training gynecological surgeons in a risk-free environment. The second is a personal medical device used by women to manage the symptoms of pelvic organ prolapse by providing internal support.
2. Is the personal Gynecube device safe to use?
Yes, the personal Gynecube device is made from medical-grade, body-safe materials. It is designed for ease of use and comfort. However, it is always recommended to consult with a healthcare provider before starting any new treatment for pelvic prolapse to ensure it is the right choice for you.
3. How realistic is the Gynecube training simulator?
The simulator is extremely realistic. It uses high-fidelity models that mimic human tissue and incorporates haptic feedback technology, which allows surgeons to feel the tactile sensations of performing a procedure, such as tissue resistance and suture tension.
4. Can the Gynecube simulator mimic surgical complications?
Yes, one of its most valuable features is the ability to simulate a wide range of complications, such as unexpected bleeding or rare anatomical variations. This prepares trainees to manage difficult, high-stakes situations in a controlled setting, which significantly improves their real-world readiness.
5. Is the personal Gynecube a permanent cure for prolapse?
The personal Gynecube is a supportive device designed to manage symptoms and improve quality of life; it is not a cure for the underlying condition of weakened pelvic tissues. It works by providing physical support to the pelvic organs. For permanent solutions, surgical options would need to be discussed with a specialist.